KINGSTON, R.I. – Oct. 19, 2023 – The opioid epidemic has continued unabated since its start in the 1990s. According to the Centers for Disease Control and Prevention, nearly 280,000 people in the U.S. died from overdoses involving prescription opioids from 1999 to 2021. In 2021, overdoses involving opioids—including prescription opioids, heroin, and synthetic opioids such as fentanyl—killed more than 80,000 people, 10 times the number of those killed in 1999.
The drug buprenorphine has been a major weapon in decreasing non-prescribed use, cravings and overdose deaths for those with opioid-use disorder.

Backed by a $2.6 million federal grant, a team of researchers from the University of Rhode Island and the UMass Chan Medical School is developing a wearable device that would be able to detect if people are taking their medication for opioid-use disorder, increasing the likelihood they would remain in treatment and preventing overdose deaths.
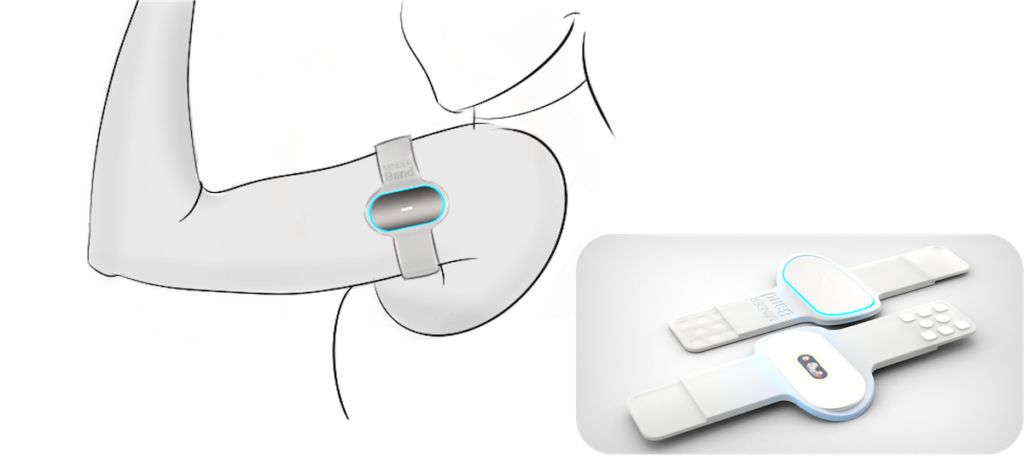
The upper-arm device—called the MINDER-band—will use a sensor system that employs machine learning to monitor physiological changes in people with opioid-use disorder to accurately identify buprenorphine use, withdrawal or relapse.
“We identified a clinical problem with buprenorphine, a medication for opioid-use disorder that works really well if people take it,” said Stephanie Carreiro, M.D., Ph.D., associate professor of emergency medicine at UMass Chan and principal investigator on the development of the device. “For several reasons, people stop taking it, develop opioid withdrawal and go back into the same routines they were in before.”
“The band will measure physiological signals and use that information to determine if the person has taken the buprenorphine,” said Krishna Venkatasubramanian, URI professor of computer science and statistics and director of the Accessible and Socially Aware Technologies Lab. “Normally this is learned from a blood or urine test. We are trying to do this non-invasively. If we can learn in real time or close to real time that the person has gone off their medication and get that information to clinicians, interventions can be brought in to help the person.”
The four-year project, which is funded by the National Institutes of Health’s National Institute of Biomedical Imaging and Bioengineering, is bringing together researchers from vastly different disciplines.
At URI, Venkatasubramanian along with Kunal Mankodiya and Dhaval Solanki, professors of electrical, computer and biomedical engineering who direct URI’s Wearable Biosensing Lab, are developing the device and its application. At UMass Chan, Dr. Carreiro and David Smelson, Pys.D., professor of medicine and director of the Center of Excellence in Addiction, will oversee clinical testing, patient recruitment and data collection for the MINDER system.
“This project is an excellent example of interdisciplinary work among technical and clinical domains that we normally do not think of coming together,” said Mankodiya. “All of us come together with the same mission of building helpful health technologies. We don’t want things to happen only in the lab. We really want to bring it out of the lab to help populations that really need it.”
The MINDER-band will use small sensors to measure such physiological signals as heart rate, body temperature and perspiration to determine if the person has taken buprenorphine, missed the dose, is in withdrawal, or relapsed. It will use machine-learning algorithms to answer that question and a system to upload those findings so they are available to clinicians.
“The signals we are looking for are well known,” said Solanki. “But putting them together in a small setup like an armband and acquiring correct physiological signals from that tiny setup is a challenge that we are trying to solve. We want to make sure the signals we are capturing using these tiny electronics are equivalent to a medical-grade signal.”
A big part of the puzzle, said Venkatasubramanian, is creating a baseline data set for people with opioid-use disorders. “We need the data and a label or ground truth that tell you what this physiological data represents,” he said. “Does it represent taking buprenorphine? Does it represent a relapse? Or does it represent something else?”
But no such data set exists for the community—specifically people with opioid-use disorder who are taking buprenorphine, Solanki said. “When all of us came together, we realized that there was no pre-data set related to this specific population from which we can learn and create models,” he said. “So there is a dire need to collect this type of data and curate that.”
Design of the armband will rely greatly on input from clinicians, social workers, and people with opioid-use disorders. This month, Venkatasubramanian’s ASSET lab and UMass Chan researchers began meeting with members from those groups to effectively integrate the new device into the lives of the people who will use it. Such feedback could affect design elements big and small, such as data collection, placement of the band, and charging the device.
“Almost everything affects design,” he said. “We need to understand the lived experience of all these folks.”
The ASSET lab has several projects at the intersection of accessibility, human computer interaction, and machine learning applied to understand and address socio-technical problems focused on marginalized populations, such as people with disabilities and people with opioid-use disorders.
In the URI Wearable Biosensing Lab, Mankodiya and Solanki have been exploring numerous projects with similarities to the MINDER-band development, including a glove with sensors for Parkinson’s patients and a chest-band sensor to noninvasively monitor infants in the neonatal intensive care units in collaboration with clinicians in and around Rhode Island.
“I’m looking forward to developing a new type of smart wearable device,” Mankodiya said. “The device we are creating will improve adherence. But questions like how often they are wearing the band or are they really wearing it or not—all these are going to be really interesting for monitoring usability. Our learning from other projects will give us a head start. However, it is always a new game.”

